Here We Go Again…Another article about low back pain? Well, I guess I should start off like every other piece written about low back pain. According to the Journal of Orthopedic and Sports Physical Therapy, 80% of the population will, at some point in their lives, experience some kind of low back pain. There, I said it. So what can I possibly tell you about low back pain that you haven’t heard already? Well, I have seen living proof of the debilitating effects of low back pain on a regular basis as people from all walks of life continue to come into my physical therapy office with low back pain. In fact, it’s probably the most common injury or diagnosis that I treat, but this article isn’t necessarily about low back pain. It is focused on one cause of LBP that people seem to equate to the worst of the worst: the dreaded, despised and highly feared herniated disc! In this article, I will debunk several myths and hopefully put you at ease if you hear or ever heard your doctor tell you that you are a victim of the herniated disc!
Is My Disc Herniated, Bulged, Slipped…?
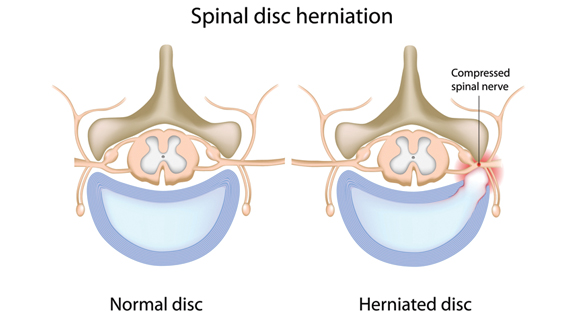
I’ve heard just about every adjective to describe a lumbar disc injury: slipped, deranged, protruded, bulged, broken, etc. First, let me simplify the definition. If you’ve been to my physical therapy office, you may have heard me use the jelly donut analogy. Think of a disc as a jelly donut that sits between two vertebrate of the spine. It absorbs shock, provides cushioning and most importantly, provides the joint with a surface to move on. Ideally, we want the jelly to stay in the center of the donut. Now, imagine the jelly inside the donut pushing out against the side of the donut, but not breaking through the surface, causing a bulge. Now, imagine the jelly, bursting through the side of the donut and protruding outside of the surface. We call that a herniation (of a disc that is). I hope you follow. If not, at least you now know about my affinity for donuts! Either type of disc protrusion can elicit an inflammatory response from the brain, which, in turn, may cause pain and even compression of a nerve in the spine. This is a cause of what is commonly known as sciatica. I am not trying to say that disc injuries and sciatica can’t be serious or debilitating injuries. I have even sent a couple of patients to pursue surgical intervention because of the severity of their injuries. These particular cases could not be treated conservatively with PT. However, these cases are extremely rare. In most cases, disc herniations can be managed conservatively by doing exercises and utilizing manual therapy techniques that help alleviate the deep inflammation and hence take away the pain and even prevent further episodes of pain.
“I Can’t Wait To Get My MRI!”
According to the Journal of Orthopaedic and Sports Physical Therapy, 90% of healthy individuals over the age of 60 have findings of bulging discs on MRI. This is a very interesting statistic for me and here is why it is for you too. Typically, before a patient with low back pain comes into my office, she has already seen her physician, had an MRI done and waited a few days to a week for the results. I see this as a waste of time because MRIs don’t always tell the whole story. Lumbar disc injuries are very common even in healthy individuals without back pain. MRIs are too often used as a way to guide treatment. It is possible to be pain free and positive MRI for a disc injury just as it is possible to have severe LBP and negative MRI results. Good clinicians don’t need imaging to treat injuries properly; which is why you need a good clinician if you have back pain. However, an MRI may be needed if proper conservative treatment does not elicit noticeable results in 2-3 weeks. An MRI can help rule out other serious issues that can cause numbness and weakness in the legs such as cancer, high-grade spondylolysthesis or a spinal fracture. A good physical therapist will be able to identify more serious issues and will know when to refer you back to your doctor. If you are a patient with chronic, episodic low back pain with radiating pain into one leg and you have just spent 3 weeks undergoing diagnostic imaging, doctor visits and a lot of rest, you have just wasted a good amount of time. Time that could have been spent on getting physical results not just test results and let’s not mention the healthcare costs associated with over-MRI-testing (at about $1,000 a pop) which directly come back to you, the patient, in the form of higher co-pays and premiums.
“I Have a Herniated Disc, Therefore I Need Surgery.”
While there have been many great technological advances in the field of spinal surgery in the past 10 to 15 years, results can often be misleading. Failed Back Surgery Syndrome (FBSS) is a chronic pain condition that has considerable impact on the patient as well as the healthcare system. FBSS involves having multiple surgeries for low back pain with each additional surgery having a significantly lower possible success rate than the last. Don’t get me wrong, I have treated many patients who underwent successful low back surgeries. I have rehabilitated and helped many more patients with low back pain avoid surgery with physical therapy intervention. Common PT interventions for low back pain include but are not limited to, soft tissue mobilization (massage), therapeutic exercise to address muscle imbalances, poor core and lumbar stabilization, as well as various other therapeutic activities in accordance with patients’ work or recreational activities. However, it should be noted that physical therapy is not an easy route to take. It involves hard work, dedication, learning, persistence and a knowledgeable and skilled therapist. Even if a patient decides to go through with surgery, she will still need skilled physical therapy before and after the surgical intervention to ensure positive results, avoid chronic back pain and even prevent FBSS. Therefore, before you consider lumbar surgery, make sure you speak to your spine specialist or orthopedic doctor about giving a good physical therapist a shot. If you are currently receiving PT and are ONLY getting modalities such as electrical stimulation, ultrasound, moist heat and a couple of exercises that never progress, come see me because that is NOT good therapy!
Conclusion
It is not uncommon for a patient new to PT to enter my office with a folder full of papers, a limp from back pain and the look of severe depression and tell me, “My doctor says I have herniated discs!” It is also not uncommon for me to look them in the eye after hearing how alarmed and scared they are and say, “It’s not that bad” and continue to explain some of the things I have just written about in the above paragraphs. What I always tell my patients is that herniated or bulging discs are not a disease. They occur through the process of degeneration of the spine. Just like the brakes on your car or the shoes on your feet, lumbar discs suffer wear-and-tear. By utilizing physical therapy, a patient with disc injury can build up all the surrounding muscles of the spine and hips, decrease muscle spasm and essentially return to functional activities she may have enjoyed before pain. This article was intended to give the reader inside information into the world of herniated discs but it cannot cover all myths and questions one may have. Hopefully, it will make you question your beliefs about herniated or bulging discs, get off the couch, get out of doctors’ offices and get you started on the road to recovery.
Doctor Ryan Martin is a Doctor of Physical Therapy and Co-Founder of ProMet Physical Therapy P.C. He practices at the Middle Village office and can be reached for comments and questions at Ryan@ProMetpt.com; for more information, visit www.prometpt.com