I was around 10 when I was offered honeydew melon to try for the first time. It was late August, the time when many local fresh fruits were in season. After a few bites, my mouth began to itch, and my throat got sore. My folks though I was getting sick. Only after I tried the melon a second time did I realized that I wasn’t sick and something else was going on – one of many childhood experiences that drove me to study allergy.
Oral Allergy syndrome, also known as Pollen-Food syndrome, is a type of food allergy to raw fruits, vegetables, nuts and seeds. It occurs in many patients with seasonal allergic rhinitis. The immune reaction to certain pollens is confused by the body with proteins in raw fruit and vegetables producing a local allergic response, namely swelling and itching. This is called a class 2 food allergy because the allergy occurs after the person has been exposed to and becomes allergic first to inhaled pollen.
Symptoms include an itchy, scratchy throat or swollen tongue and throat that resolve over 20 minutes or so. Digestive juice and acid break down the allergen and the reaction resolves. Investigators have discovered that the protein that causes the reaction is present only in raw fruit and vegetables and can be neutralized by heating or cooking. Apple pie, peach pie or canned fruit? No problem man!
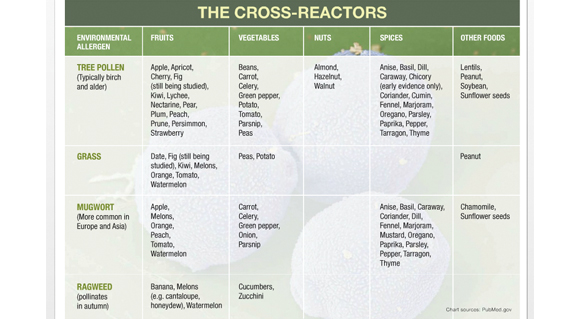
The cross-reactivity between pollen and fruit falls into specific groups. Apples, peaches, carrots, celery, and hazelnuts have high incidence of cross-reactivity with birch pollen and springtime allergies. Melons, bananas and cucumbers cause symptoms in grass and ragweed sufferers which are fall allergies. Ripe, tasty fruit may produce more severe symptoms than unripe fruit.
testing for this syndrome
Recognizing and testing for this syndrome requires the expertise of an allergy specialist. Commercial skin testing extracts and blood tests will often be negative because they cannot test the allergen that is present in fresh produce. Fresh food extracts are more helpful. Recent advances in allergy testing allow for more specific components within each allergen to be evaluated. This is helpful because allergen components that cross-react are less likely than food specific allergens to cause a severe anaphylactic reaction. In general, anaphylaxis in this condition is very rare.
Cases of severe reactions to raw fruit have been associated with nuts, peaches, apples and celery. Drinking alcohol or strenuous exercise may amplify the oral allergic reaction and produce gastrointestinal symptoms and anaphylaxis.
Fortunately, most cases of oral allergy are mild and rarely lead to severe symptoms. Simple avoidance and replacement with other fruits or vegetables is preferable. Tropical fruits are usually a safe alternative. Peeling, cooking or microwaving may decrease the heat sensitive allergen to a tolerable level.
It took 20 years for me discover that I wasn’t ill – it was just Oral Allergy Syndrome.
Dr. Gontzes is board certified in Allergy & Immunology and has 32 years of experience.He is a resident of Middle Village and a member of the Juniper Park Civic Association.
Peter Gontzes MD
9231 57th Ave
Elmhurst, NY 11373
(718) 592-1731